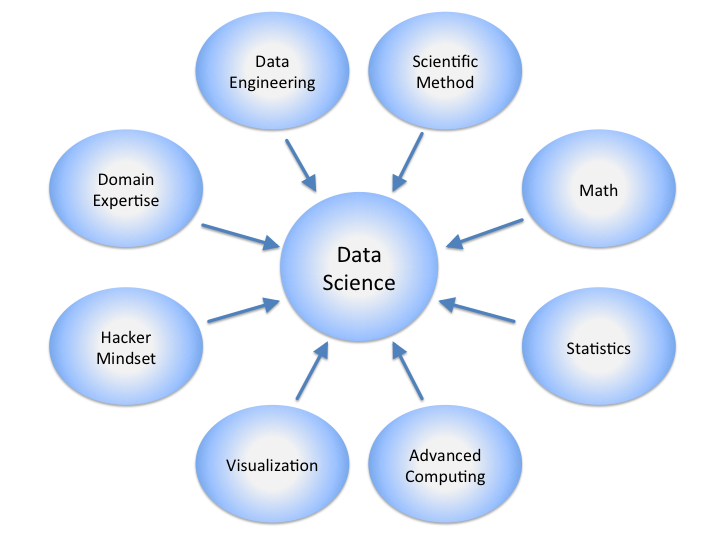
A well-written framework on Stanford Social Innovation Review describes three distinct forces of transforming a practice.
An agitator brings the grievances of specific individuals or groups to the forefront of public awareness. An innovator creates an actionable solution to address these grievances. And an orchestrator coordinates action across groups, organizations, and sectors to scale the proposed solution.
The key observation is that transformation requires all three in harmony. In medicine, the voices of agitators frequently meet top-down repression or with the silence of the leadership. “This is just the way we’ve always done it,” they might say.
The Stanford article focuses on building a team consisting of people in all three domains in order to bring about social innovation. In medicine, practices tend to be resistant to change partly due to the higher stakes but also due to the highly regulated climate of modern health care. (This is not necessarily good or bad – it just is.)
Although medicine often places more weight on orchestration – coordination of interdisciplinary care to benefit patient health – it stands to reason that a healthy dose of the other two is also necessary. If you see yourself as an agitator, know that a thorough understanding of stakeholder analysis can help you better differentiate between a simple inconvenience and an opportunity to create value. If you are an innovator, your strength may lie in an intuitive visualization of connections between disparate organizational units. Know that what seems obvious to you is probably opaque to others. In the end:
Agitation without innovation means complaints without ways forward, and innovation without orchestration means ideas without impact.